Traditionally, spine surgery is performed as an open surgical procedure. This involves a relatively long incision to allow the surgeon to directly visualize and access the spine. Recent developments and technological advances have allowed many spine conditions to be treated with minimally invasive techniques.

What is Minimally Invasive Spine Surgery?
Minimally invasive spine surgery (MISS) allows surgeons to access deep spinal structures through small or minimally invasive incisions. Minimally invasive surgery (MIS) is possible with the use of fluoroscopic (real-time x-ray) image guidance that helps the surgeon navigate through small openings. The result is smaller incisions with less soft tissue manipulation and less blood loss compared to conventional open surgery. Smaller incisions mean more comfortable and faster recovery periods. Patients treated with minimally invasive spine surgery often require less post-operative pain medication and are likely to return to their normal daily activities sooner. Furthermore, patients often do not require inpatient hospital admissions as most minimally invasive spinal procedures are performed on an outpatient basis.
Not all spine surgery procedures can be performed using minimally invasive surgery. Often, it is important to have direct visualization and access to the delicate neural and vascular structures while performing spinal surgery. Sometimes the patient’s condition can result in significant displacement of important nerves that control motor and/or sensory function.

Damage to these nerves within the spinal column may result in permanent neurologic deficit or paralysis. Therefore, it is important that your surgeon acknowledge which procedures are most appropriate for minimally invasive spine surgery and which are not.
When Is Spine Surgery Necessary?
Spine surgery is typically recommended when a period of nonsurgical treatment has not relieved the painful symptoms caused by your back problem. Examples of nonsurgical treatment may include pain medication, physical therapy, epidural steroid injections, chiropractic manipulation, and acupuncture. However, other spinal conditions that cause acute onset of weakness, loss of sensation, or bowel and bladder dysfunction may require immediate surgical intervention. It is therefore important that your health care provider determine when surgical intervention is immediately required or if conservative therapy should be initially pursued.
Open Spine Surgery Procedure
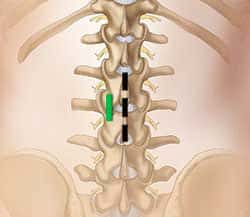
This illustration below shows a common incision site in the lower back that is used for some traditional open spine surgeries. A 1-2 inch skin incision (black line) is made down the middle of the back. Muscles overlying the vertebrae are retracted to one side. For minimally invasive spinal surgery, a small stab entry (green line) is made in the skin just off midline.
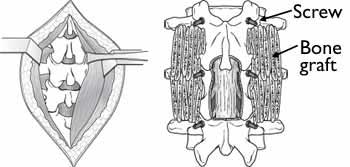
In the image to the right, (Left) In open surgery, muscles and soft tissue surrounding the spinal column are retracted laterally to reveal the damaged area. (Right) After removing portions of the bone, bone graft material and screws are placed along the sides of the vertebrae.
Minimally Invasive Spine Surgery Procedure
A tubular retractor is used to create a passageway for the surgeon to reach the problem area of the lower back. MIS surgery fusions and decompression procedures (such as discectomy and laminectomy) are performed with special tools called tubular retractors. During the procedure, a small incision is made and a small tubular retractor is inserted through the skin and soft tissues down to the spinal column.

Larger diameter tubular retractors are subsequently inserted over the initial retractor. This process creates a tunnel to the small area where the problem exists in the spine. The tubular retractor holds the muscles open and is kept in place throughout the procedure. Small fiber optic lights are used to illuminate the area at the distal end of the tubular retractor.
The surgeon accesses the spine using small elongated instruments that fit through the center of the tubular retractor. Any bone or disk material that is removed exits through the retractor, and any devices necessary for fusion such as screws or rods are inserted through the tubular retractor. Some surgeries require more than one retractor and one or several small incisions. In order to see where to place the incision and insert the retractor, the surgeon is guided by fluoroscopy. This method displays real-time x-ray images of the patient’s spine on a screen throughout the surgery. The surgeon may also use an operating microscope to magnify the view through the retractor.
At the end of the procedure, the tubular retractor is removed and the muscles return to original position. This limits the muscle damage that is more commonly associated with open surgeries.
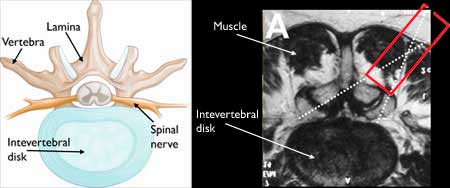
In the image above (Left) An illustration showing a cross-section view of a healthy intervertebral disk. (Right) A cross-section magnetic resonance imaging (MRI) scan of the anatomy surrounding an intervertebral disk.
The solid red rectangle shows the placement of the tubular retractor through the muscle and the dotted lines indicate the positioning of small surgical instruments.
Is Anesthesia Used During Minimally Invasive Spine Surgeries?
Most patients are placed under general anesthesia during MIS surgery procedures. However, some procedures may be performed using regional anesthesia or spinal blocks which allows patients to be awake but without any sensation in the area of the surgery.
Common Minimally Invasive Spine Surgeries
Common minimally invasive spine surgery procedures include discectomies or decompression surgery and spinal fusion. Decompression procedures relieve pressure on nerves caused by degenerative bone and/or herniated discs. Spinal fusion is a technique used to restore the integrity of the spinal column that has been compromised.
MIS Lumbar Discectomy
A herniated disk in the lower back that pinches a nerve may cause severe leg pain, numbness, or weakness. To surgically relieve these symptoms, the part of the disc that is compressing the neural elements is removed. This procedure is called a discectomy. For the surgery, the patient is positioned face-down and a small incision (approximately 1 inch) is made over the location of the herniated disk. The surgeon inserts the retractor and removes a small amount of the bone in order to gain access to the disc herniation. The surgeon carefully retracts the nerve and removes the damaged disc.
MIS Lumbar Fusion
A common MIS fusion is the transforaminal lumbar interbody fusion (TLIF). In an MIS TLIF, the patient is positioned face-down and the surgeon places one retractor on either side of the spine. This approach prevents disruption of the midline ligaments and bone as well as the adjacent spinal nerve. Using the two retractors, the surgeon can remove the lamina and the disc, replace bone graft into the disc space and place screws or rods to secure the construct.
Recovery After Minimally Invasive Spine Surgery
Minimally invasive spine surgery can shorten hospital stays. Some patients may go home the day of surgery. Other patients may require a 1-3 day hospital stay. Because minimally invasive techniques do not disrupt muscles and soft tissues to a significant degree, it is believed that post-operative pain is less compared to pain after traditional, open surgeries. You should still expect to feel some discomfort, however, advancements in pain control now make it easier for your doctor to manage and relieve pain.
To help you regain strength and speed your recovery, your doctor may recommend physical therapy. This will depend on the procedure you have had and your general physical condition. Specific exercises will help you become strong enough to return to work and daily activities.
If you have had a fusion procedure, it may be several months before the bone is solid, although your comfort level will often improve much faster. During this healing time, the fused spine must be kept in proper alignment and you may be instructed to wear a brace. You will be taught how to move properly, reposition, sit, stand, and walk.
How Long Will It Take To Return To Normal Activities After MIS Surgery?
How long it will take to return to your daily activities after MIS surgery depends upon your individual procedure and condition. Your surgeon will evaluate you after your surgery to make sure that your recovery is progressing as expected.
Why Choose Dr. Lipani For Your Minimally Invasive Spinal Surgery?
At Princeton Neurological Surgery, Dr. Lipani is a board certified fellowship trained neurosurgeon and specialist in minimally invasive spinal surgery in New Jersey. Dr. Lipani treats patients from around the world as well as locally from Princeton, New Brunswick, Hopewell, Pennington and communities throughout Somerset, Middlesex, Ocean, Burlington, Monmouth and Mercer Counties for all types of spinal conditions. Dr. Lipani offers both conventional open and minimally invasive approaches, tailored to the needs of each patient.

Risks Of Minimally Invasive Spine Surgery
As with any operation, there are potential risks associated with MIS surgery. Complications of MIS surgery are similar to open spinal surgery; however, some studies show a reduced infection rate for MIS surgery. It is important to discuss these risks with your neurosurgeon before your procedure.
- Infection.
Antibiotics are regularly given to the patient before, during, and often after surgery to lessen the risk of infections. - Bleeding.
A certain amount of bleeding is expected, but this is not typically significant. - Pain at graft site.
If your surgeon chooses to obtain bone from your hip or other areas you may experience persistent pain at the bone graft site. - Recurring symptoms.
Some patients may experience a recurrence of their originalsymptoms. - Pseudarthrosis.
Patients who smoke, have diabetes, and/or renal failure are more likely to develop a pseudarthrosis or failed fusion. This is a condition where there is not enough bone formation. If this occurs, a second surgery may be required in order to obtain a solid fusion. - Nerve damage.
It is possible that the nerves or blood vessels may be injured during these operations. These complications are very rare. - Blood clots.
Another uncommon complication is the formation of blood clots in the legs. These pose significant danger if they break off and travel to the lungs. Blood clots often occur due to prolonged periods of immobility which is unusual with MIS surgery.
Schedule a Consultation
For state-of-the-art spine surgery treatment, or to learn about lumbar disc surgery, surgery for spinal stenosis, spinal fusion procedures, or other procedures, call us to schedule a consultation at our offices in Hamilton, Bridgewater, or Toms River, New Jersey.